PRP會加速放射線照射後的皮膚再生、恢復皮脂腺功能、增加膠原蛋白產生、減少皮膚水分流失
PRP會加速放射線照射後的皮膚再生、恢復皮脂腺功能、增加膠原蛋白產生、減少皮膚水分流失
對嚴重、急性放射性皮膚損傷的治療選擇很有限,而PRP可改善皮膚傷口癒合,可藉由AKT訊息傳遞,而增強角質細胞K14的功能,加速放射線照射後的皮膚再生。對於臨床的放射性傷口癒合有重大助益。
PRP科技新知 - PRP會加速放射線照射後的皮膚再生、恢復皮脂腺功能、增加膠原蛋白產生、減少皮膚水分流失
研究背景:
各種形式的放射線都會造成皮膚損傷。然而,針對嚴重、急性放射性皮膚損傷的治療選擇很有限。目前已知PRP可改善皮膚傷口癒合,但PRP對於高劑量放射線照射的效果仍知之甚少。
研究方法:
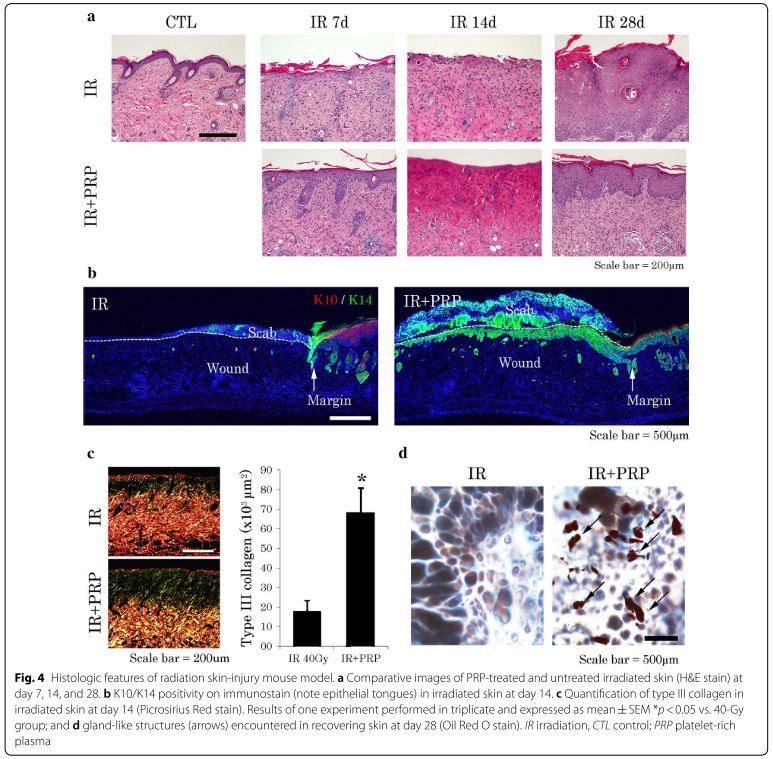
使用小鼠背部皮膚進行局部照射40格雷(Gy),並使用伽馬射線5格雷來照射HaCaT細胞(這是一種來自於成年人類的永生化角質形成細胞的細胞株)用於研究 PRP的再生功能。利用評估傷口大小、組織學特徵、免疫染色、西方墨點法和經皮水分流失(TEWL)來評估PRP對於皮膚的益處。為了評估PRP對於輻射傷口的癒合狀況與角質形成細胞的分子影響,我們評估了AKT訊息傳遞路徑。
結果:
儘管經輻射受損的HaCaT細胞癒合能力下降,但在照射後的HaCaT細胞和皮膚組織中,角質細胞14(Keratin 14, K14)的表現量升高。使用PRP後,可以經由增強AKT訊息傳遞恢復皮膚癒合能力。在我們的小鼠模型中,使用PRP可證實以下結果:(1)增加放射性皮膚炎的皮膚癒合能力;(2)激活AKT訊息傳遞,改善角質細胞K14的遷移和增殖;(3) 增加角質細胞K10與皮脂腺的內披蛋白表現能力;(4)減少經皮水分流失TEWL,加強皮膚屏障功能。
結論:
PRP可藉由AKT訊息傳遞,而增強角質細胞K14的功能,加速放射線照射後的皮膚再生。對於臨床的放射性傷口癒合有重大助益。
原文摘要:
BACKGROUND: The skin is impacted by every form of external radiation therapy. However, effective therapeutic options for severe, acute radiation-induced skin reactions are limited. Although platelet-rich plasma (PRP) is known to improve cutaneous wound healing, its effects in the context of high-dose irradiation are still poorly understood.
METHODS: We investigated the regenerative functions of PRP by subjecting the dorsal skin of mice to local irradiation (40 Gy) and exposing HaCaT cells to gamma rays (5 Gy). The cutaneous benefits of PRP were gauged by wound size, histologic features, immunostains, western blot, and transepithelial water loss (TEWL). To assess the molecular effects of PRP on keratinocytes of healing radiation-induced wounds, we evaluated AKT signaling.
RESULTS: Heightened expression of keratin 14 (K14) was documented in irradiated HaCaT cells and skin tissue, although the healing capacity of injured HaCaT cells declined. By applying PRP, this capacity was restored via augmented AKT signaling. In our mouse model, PRP use achieved the following: (1) healing of desquamated skin, acutely injured by radiation; (2) activated AKT signaling, improving migration and proliferation of K14 cells; (3) greater expression of involucrin in keratin 10 cells and sebaceous glands; and (4) reduced TEWL, strengthening the cutaneous barrier function.
CONCLUSIONS: Our findings indicate that PRP enhances the functions of K14 cells via AKT signaling, accelerating the regeneration of irradiated skin. These wound-healing benefits may have merit in a clinical setting.
文章出處: Lee J, Jang H, Park S, Myung H, Kim K, Kim H, Jang WS, Lee SJ, Myung JK, Shim S: Platelet-rich plasma activates AKT signaling to promote wound healing in a mouse model of radiation-induced skin injury. J Transl Med 2019, 17(1):295.
研究背景:
各種形式的放射線都會造成皮膚損傷。然而,針對嚴重、急性放射性皮膚損傷的治療選擇很有限。目前已知PRP可改善皮膚傷口癒合,但PRP對於高劑量放射線照射的效果仍知之甚少。
研究方法:
使用小鼠背部皮膚進行局部照射40格雷(Gy),並使用伽馬射線5格雷來照射HaCaT細胞(這是一種來自於成年人類的永生化角質形成細胞的細胞株)用於研究 PRP的再生功能。利用評估傷口大小、組織學特徵、免疫染色、西方墨點法和經皮水分流失(TEWL)來評估PRP對於皮膚的益處。為了評估PRP對於輻射傷口的癒合狀況與角質形成細胞的分子影響,我們評估了AKT訊息傳遞路徑。
結果:
儘管經輻射受損的HaCaT細胞癒合能力下降,但在照射後的HaCaT細胞和皮膚組織中,角質細胞14(Keratin 14, K14)的表現量升高。使用PRP後,可以經由增強AKT訊息傳遞恢復皮膚癒合能力。在我們的小鼠模型中,使用PRP可證實以下結果:(1)增加放射性皮膚炎的皮膚癒合能力;(2)激活AKT訊息傳遞,改善角質細胞K14的遷移和增殖;(3) 增加角質細胞K10與皮脂腺的內披蛋白表現能力;(4)減少經皮水分流失TEWL,加強皮膚屏障功能。
結論:
PRP可藉由AKT訊息傳遞,而增強角質細胞K14的功能,加速放射線照射後的皮膚再生。對於臨床的放射性傷口癒合有重大助益。
原文摘要:
BACKGROUND: The skin is impacted by every form of external radiation therapy. However, effective therapeutic options for severe, acute radiation-induced skin reactions are limited. Although platelet-rich plasma (PRP) is known to improve cutaneous wound healing, its effects in the context of high-dose irradiation are still poorly understood.
METHODS: We investigated the regenerative functions of PRP by subjecting the dorsal skin of mice to local irradiation (40 Gy) and exposing HaCaT cells to gamma rays (5 Gy). The cutaneous benefits of PRP were gauged by wound size, histologic features, immunostains, western blot, and transepithelial water loss (TEWL). To assess the molecular effects of PRP on keratinocytes of healing radiation-induced wounds, we evaluated AKT signaling.
RESULTS: Heightened expression of keratin 14 (K14) was documented in irradiated HaCaT cells and skin tissue, although the healing capacity of injured HaCaT cells declined. By applying PRP, this capacity was restored via augmented AKT signaling. In our mouse model, PRP use achieved the following: (1) healing of desquamated skin, acutely injured by radiation; (2) activated AKT signaling, improving migration and proliferation of K14 cells; (3) greater expression of involucrin in keratin 10 cells and sebaceous glands; and (4) reduced TEWL, strengthening the cutaneous barrier function.
CONCLUSIONS: Our findings indicate that PRP enhances the functions of K14 cells via AKT signaling, accelerating the regeneration of irradiated skin. These wound-healing benefits may have merit in a clinical setting.
文章出處: Lee J, Jang H, Park S, Myung H, Kim K, Kim H, Jang WS, Lee SJ, Myung JK, Shim S: Platelet-rich plasma activates AKT signaling to promote wound healing in a mouse model of radiation-induced skin injury. J Transl Med 2019, 17(1):295.

