
蘆薈"無法"預防放射性皮膚炎的發生率和嚴重度
蘆薈"無法"預防放射性皮膚炎的發生率和嚴重度
放射治療所引起的皮膚炎(是一種常見且有時很嚴重的副作用,很多人誤以為蘆薈凝膠可以降低放射性皮膚炎的發生率及嚴重度,經研究證實蘆薈對放射性皮膚炎的發生率和嚴重程度沒有影響。
PRP科技新知 - 蘆薈"無法"預防放射性皮膚炎的發生率和嚴重度
研究目的:
放射治療所引起的皮膚炎(以下簡稱放射性皮膚炎)是一種常見且有時很嚴重的副作用。本文章是隨機性研究,以了解使用蘆薈凝膠是否可以降低放射性皮膚炎的發生率及嚴重度。
研究方法:
100 名新診斷的乳癌患者在放射治療期間隨機接受蘆薈凝膠或不接受蘆薈凝膠,觀察並記錄其副作用。放射治療使用 6 MV 直線加速器的光子體外照射,總劑量為 50 格雷,每天 2 格雷,每週 5 次。
研究結果:
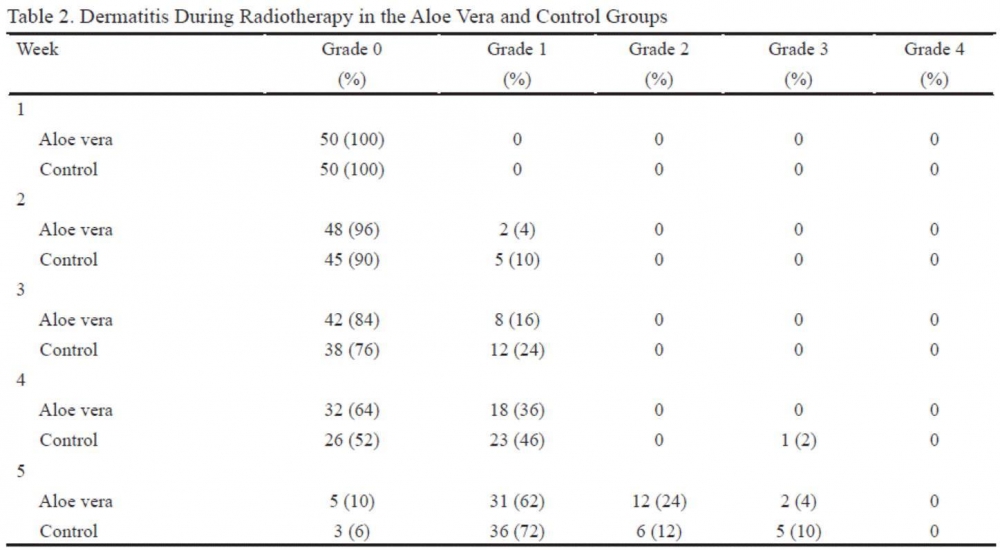
在第 2 週後兩組患者首次發現放射性皮膚炎。在蘆薈組和對照組中,2/8 名患者和 5/12 名患者在第 2 週後出現 第1級放射性皮膚炎(P 值 = 0.240)和第3級放射性皮膚炎(P 值 = 0.317)。 第 4 週後,數字為 18 例,23 例為 1 級放射性皮膚炎,只有 1 例為 3 級放射性皮膚炎(P 值 = 0.328)。 第 5 週後,蘆薈組有 31、12 和 2 名患者,對照組有 36、6 和 5 名患者分別出現 1、2 和 3 級放射性皮膚炎(P 值 = 0.488)。
結論:
在本研究中,蘆薈對放射性皮膚炎的發生率和嚴重程度沒有影響。
原文摘要:
Purpose: Radiotherapy induced dermatitis is a common and sometimes serious side effect. We conducted a randomized study to understand whether the adjunctive use of aloe vera gel might reduce the prevalence and/or severity of radiotherapy induced dermatitis.
Methods: One hundred patients with newly diagnosed breast cancer were randomized to receive aloe vera gel or nothing during adjuvant radiotherapy consisting of conventional external beam radiation using 6 MV mega voltage linear accelerator photons. The radiation portals were composed of breast fields in all patients and supraclavicular and posterior axillary fields in node positive cases. The total dose was 50 Gy with a daily fraction of 2 Gy, five fractions per week.
Results: Dermatitis was first found among patients of both groups after week 2. In the aloe vera and control groups, 2/8 patients and 5/12 patients had dermatitis grade 1 after weeks 2 (P value = 0.240) and 3 (P value = 0.317). After the 4th week, the numbers were 18 and, 23 for dermatitis grade 1 and only 1 for grade 3 dermatitis (P value = 0.328). After the 5th week, 31, 12 and 2 patients in the aloe vera group and 36, 6 and 5 of the controls had grades 1, 2 and 3 dermatitis, respectively (P value = 0.488).
Conclusion: Aloe vera exerted no positive effect on prevalence or severity of radiation dermatitis in this study.
文章出處:
N. Ahmadloo, B. Kadkhodaei, S. Omidvari, A. Mosalaei, M. Ansari, H. Nasrollahi, et al. Asian Pac J Cancer Prev 2017 Vol. 18 Issue 4 Pages 1139-1143
研究目的:
放射治療所引起的皮膚炎(以下簡稱放射性皮膚炎)是一種常見且有時很嚴重的副作用。本文章是隨機性研究,以了解使用蘆薈凝膠是否可以降低放射性皮膚炎的發生率及嚴重度。
研究方法:
100 名新診斷的乳癌患者在放射治療期間隨機接受蘆薈凝膠或不接受蘆薈凝膠,觀察並記錄其副作用。放射治療使用 6 MV 直線加速器的光子體外照射,總劑量為 50 格雷,每天 2 格雷,每週 5 次。
研究結果:
在第 2 週後兩組患者首次發現放射性皮膚炎。在蘆薈組和對照組中,2/8 名患者和 5/12 名患者在第 2 週後出現 第1級放射性皮膚炎(P 值 = 0.240)和第3級放射性皮膚炎(P 值 = 0.317)。 第 4 週後,數字為 18 例,23 例為 1 級放射性皮膚炎,只有 1 例為 3 級放射性皮膚炎(P 值 = 0.328)。 第 5 週後,蘆薈組有 31、12 和 2 名患者,對照組有 36、6 和 5 名患者分別出現 1、2 和 3 級放射性皮膚炎(P 值 = 0.488)。
結論:
在本研究中,蘆薈對放射性皮膚炎的發生率和嚴重程度沒有影響。
原文摘要:
Purpose: Radiotherapy induced dermatitis is a common and sometimes serious side effect. We conducted a randomized study to understand whether the adjunctive use of aloe vera gel might reduce the prevalence and/or severity of radiotherapy induced dermatitis.
Methods: One hundred patients with newly diagnosed breast cancer were randomized to receive aloe vera gel or nothing during adjuvant radiotherapy consisting of conventional external beam radiation using 6 MV mega voltage linear accelerator photons. The radiation portals were composed of breast fields in all patients and supraclavicular and posterior axillary fields in node positive cases. The total dose was 50 Gy with a daily fraction of 2 Gy, five fractions per week.
Results: Dermatitis was first found among patients of both groups after week 2. In the aloe vera and control groups, 2/8 patients and 5/12 patients had dermatitis grade 1 after weeks 2 (P value = 0.240) and 3 (P value = 0.317). After the 4th week, the numbers were 18 and, 23 for dermatitis grade 1 and only 1 for grade 3 dermatitis (P value = 0.328). After the 5th week, 31, 12 and 2 patients in the aloe vera group and 36, 6 and 5 of the controls had grades 1, 2 and 3 dermatitis, respectively (P value = 0.488).
Conclusion: Aloe vera exerted no positive effect on prevalence or severity of radiation dermatitis in this study.
文章出處:
N. Ahmadloo, B. Kadkhodaei, S. Omidvari, A. Mosalaei, M. Ansari, H. Nasrollahi, et al. Asian Pac J Cancer Prev 2017 Vol. 18 Issue 4 Pages 1139-1143

